
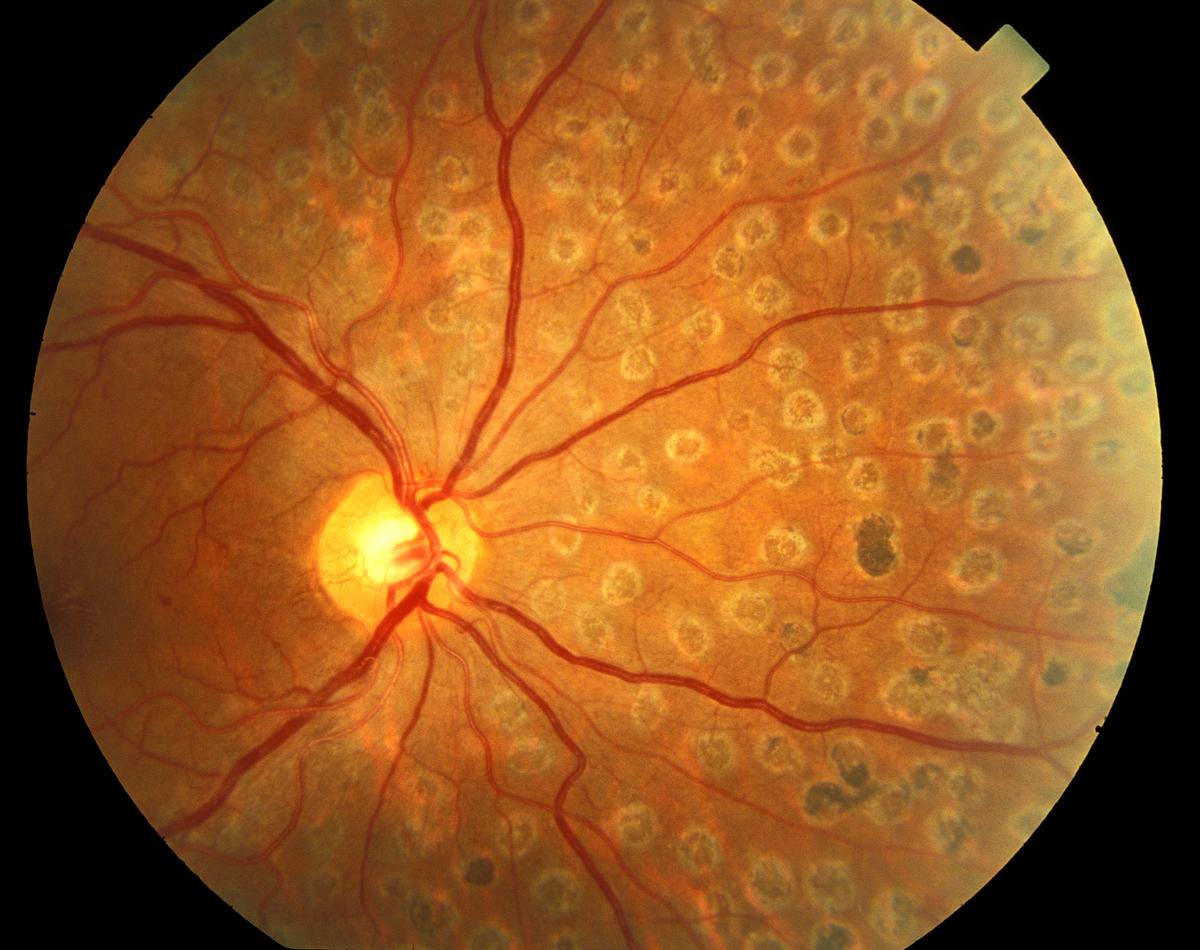
The patient is placed in a seated position, and the chin placed on the chin-rest. Slit lamp: The laser is attached to the typical ophthalmic slit lamp and the laser energy is delivered in a coaxial fashion. PRP is typically delivered through either a slit lamp system or laser indirect ophthalmoscope (headlamp/BIO). By destroying the largely unused, ischemic extramacular retina, PRP reduces the area of ischemic tissue, which in turn reduces total vascular endothelial growth factor (VEGF) production in the eye and thereby reducing the impetus for neovascularization. Classically, approximately 1000-2000 micro-burns are made on the retina. Over time, these areas of thermally damaged tissue eventually scar and become more heavily pigmented, leaving visible laser scars at the level of the RPE. Thermal burns denature tissue protein which leads to local retinal cell death and coagulative necrosis. Laser energy is absorbed is converted to thermal energy, raising the tissue temperature approximately 20 or 30 degrees Celsius. For PRP, typically yellow, green, or red laser light is used. The retinal pigments in the RPE serve to absorb nearly all wavelengths of light. Light from the laser is absorbed by the retinal pigment epithelium (RPE), and by the underlying choroid. Laser Physics and Biological Interactions However PRP remains the mainstay of treatment for PDR.

Currently, more advanced laser delivery systems and other methods of combating diabetic retinopathy are emerging. The Early Treatment Diabetic Retinopathy Study (ETDRS), conducted shortly after the DRS, examined the effects of PRP on patients with non-proliferative diabetic retinopathy (NPDR), and determined the exact stage in the disease course at which laser therapy should be administered. As a result, xenon arc laser therapy is now largely discontinued, in favor of argon laser (or modern equivalent continuous wave millisecond laser systems). This study also set forth the first detailed treatment parameters for PDR. The study showed that that laser therapy was indeed beneficial to patients with PDR and also showed that argon lasers created less adverse effects for patients than xenon lasers while retaining similar efficacy. This study, the Diabetic Retinopathy Study (DRS) examined the effects of pan-retinal photocoagulation (PRP) through both xenon arc laser and argon laser treatments on patients with proliferative diabetic retinopathy (PDR), to determine whether it was more beneficial than no treatment at all. However, an official study to investigate the effects of laser treatment via PRP was not conducted until the 1970s. The argon laser was discovered in 1964 by William Bridges. A xenon arc laser was developed in the 1950s by the Carl Zeiss Laboratory and was used clinically in the early days of retinal therapy. Laser therapy has been used to treat many pathologies in the eye for decades. 2.4 PRP and Pharmacologic Therapy of Diabetic Retinopathy.2.2.1 Long-Duration Typical Treatment (Conventional).1.2 Laser Physics and Biological Interactions.


 0 kommentar(er)
0 kommentar(er)
